Download A4Medicine Mobile App
Empower Your RCGP AKT Journey: Master the MCQs with Us!
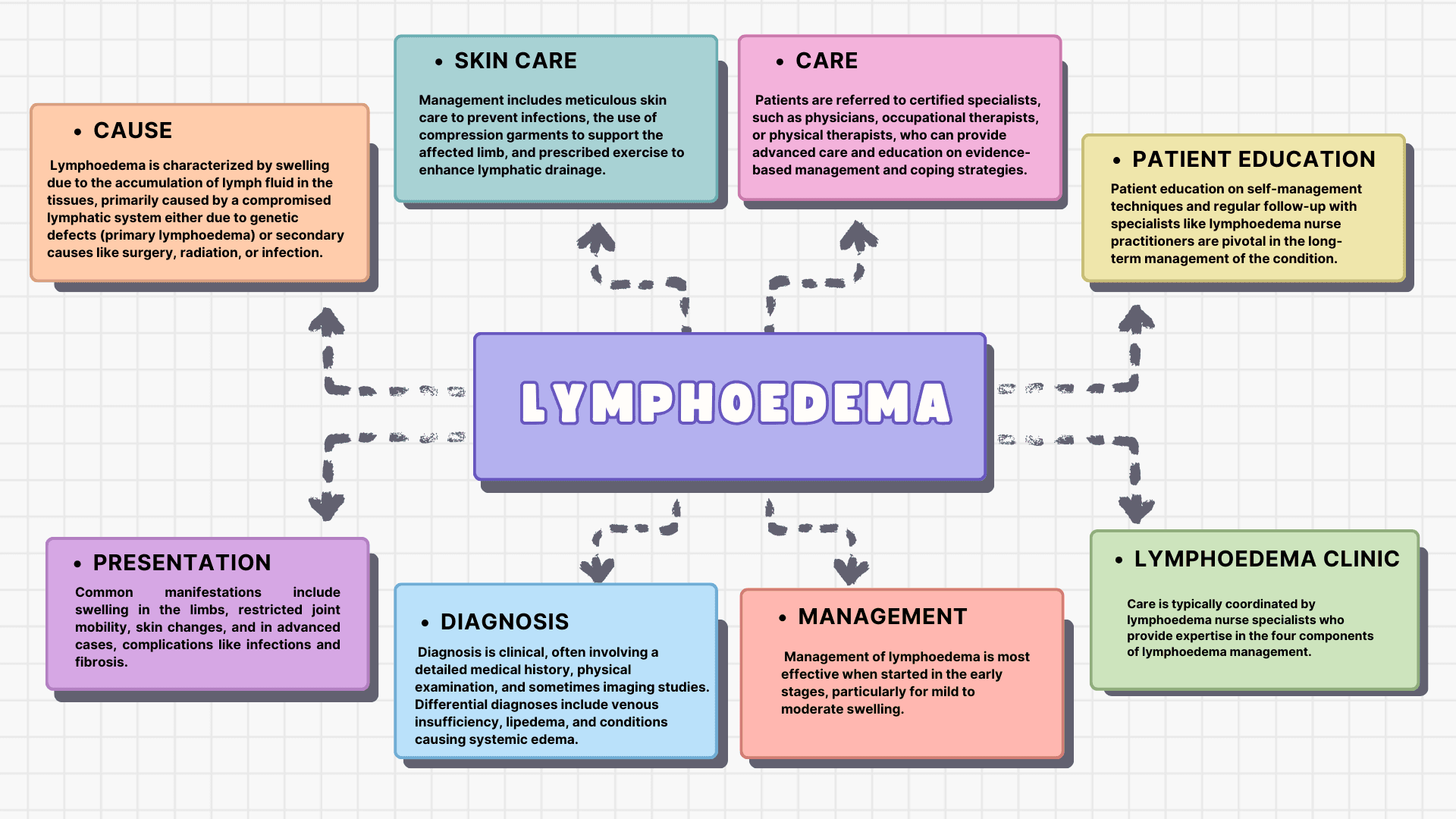
This table summarizes the complex nature of lymphoedema, from its definition, classification, causes, and progression, to the methods used for its diagnosis and differentiation from other conditions. Please also refer to our chart on peripheral oedema for a better understanding of this subject.
| Section | Subsection | Key Points |
|---|---|---|
| Lymphatic System Anatomy | Components | • Comprises initial lymphatics (capillaries), pre-collectors, collectors, lymphatic trunks, and nodes • Transports lymph containing white blood cells, triglycerides, bacteria, cell debris, water, and protein. |
| Topography | • Superficial system: Drains skin and subcutaneous areas. • Deep system: Drains muscles, joints, tendon sheaths, nerves. • Both systems connected by perforating vessels. | |
| Signs and Symptoms | General | • Distal swelling in extremities, proximal swelling in breast, chest, etc. • Restricted joint motion, skin discoloration, pain, altered sensation, limb heaviness. |
| Specific Clinical Indicators | • Dryness, increased thickness, hyperkeratosis, lymphangiomas. • Warm or hot skin, unusual darkening, nodules. • Papillomatosis presenting as cobblestone skin texture. | |
| Primary Lymphoedema | Vascular Abnormalities | • Associated with dysplasia of lymphatics, may accompany other vascular conditions like Klippel-Trenaunay-Weber syndrome, Turner syndrome. • Characterized by hyperplasia, hypoplasia, or aplasia of lymphatic vessels. |
| Secondary Lymphoedema | Oncologic and Surgical Causes | • Commonly due to cancer treatments, axillary lymph node dissection, radiation in the... |
Try our Free Plan to get the full article.